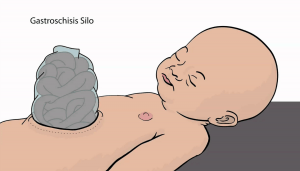
Hello everyone! I have just finished my fifth week here in Malawi. This week I spent a lot of time at Queen Elizabeth Hospital shadowing in different wards, specifically in the pediatric surgery ward, maternity ward, and audiology clinic. I also spoke with three different pediatric surgeons from Blantyre, Lilongwe, and the UK about our gastroschisis silo bags and got some great feedback from them.
Starting out with the pediatric surgery ward, I was able to observe Dr. Eric Borgstein for two days on different surgeries. He gave me a whole scrubs outfit and I got to wear crocs around for the whole day, which is always a win.
The first surgery was a lung decortication on a two-month-old baby. They took a layer of peely semi-liquid like substance off of the lungs to allow them to expand properly. This is the first surgery I had ever observed and I think the part that surprised me most was the ease with which the doctors were able to cut and make decisions right on the spot about what to do next. I had never realized that so much of a surgeon’s job is improvising on the spot when the patient’s condition presents differently once actually on the operating table than the doctor originally anticipated.
I was able to stand a few feet behind the operating table itself and ask questions to the surgeon once in awhile and even peeked over his shoulder at times when he wanted to show me something. The environment was much more relaxed than I had thought it would be. They had calm classical music playing and even carried on some light-hearted conversations whilst operating.
I saw the improvisation more so in the second surgery I shadowed in on when they were operating on a 15-year-old cancer patient. She had a burn many years ago that was never properly treated and it eventually lead to her cells multiplying uncontrollably and becoming a tumor. Dr. Borgstein had to remove the tumor and when he tried to take out her lymphnodes he found that the cancer had spread to the rest of her body. In that moment, he had to decide if he was going to continue with the surgery and try to remove more of the cancer or stop operating and close her up. Deciding to close her up, they stitched the patient and the surgery was over.
I am so in awe of the way a surgeon is able to think of all of the possible future scenarios for a patient in just a few moments, decide what they think is the best course of action, and confidentially go forward with it. I guess that is another lesson I am learning from the doctors here, not just from Dr. Borgstein, but from the OBGYNs, pediatricians, and nursing staff.
When resources are limited and costs are high, the doctors must decide how to maximize what they are given and do so without wasting materials. They also cannot second-guess themselves, which is something that I tend to do when I wonder if I am making the right decision, or not. Here, when there is neither time nor resources for a doctor to try multiple care options for a patient or weigh the pros and cons of a treatment plan at length, they trust that the decision they have made is the most educated they could make and move forward.
I also got to shadow in the maternity ward this week with some of the medical students and Dr. Sam Meja. We went on a round of the labor ward where the medical students assessed each mother, checked her for contractions or complications, and determined if she was in labor yet or not.
Most of the interaction with the mothers was done in Chichewa so I did my best to understand what they were doing through visual cues and then ask questions afterwards. I noticed that the environment in which the doctors assess mothers is very different in Malawi than in the US. In the US, everything is done very privately and the doctors and med students take permission from the mother before doing any physical check and ask questions very carefully. In Malawi, check ups are run much more publically and for this reason there were very few men in the maternity ward. I noticed mothers were rarely ever difficult about a test and overall talked very little to the doctors or asked questions.
After spending lots of time in the hospital this week I had a new found appreciation for how hard working, and for little recognition or pay, the doctors and nurses are here. I am so thankful to them for teaching me so much without even realizing they are doing so.
Over the weekend, we went to Cape Maclear at Lake Malawi and wow, was it beautiful. I have never seen such blue water in my life or a sky so clear and so filled with stars. We got to eagle watch, snorkel in the lake, and eat the freshest fish out there.
Warm Wishes,
Sajel