Part 1: Independence and Interdependence

“Thirty-five years of independence, but are we really independent?” This question rang out at the Kwa Haraba Art Gallery and Café last Wednesday, the week of Malawi’s independence day, as the first poet of the night finished his poem. The answer was not spoken but was palpable in the night air. As the evening went on, more poets performed, many of them also contemplating the fragile state of Malawi’s independence. (The only guy who claimed otherwise was a Caucasian man who sang a song whose only lyric was “One Malawi, One People”…).
Considering what we’ve seen in Malawi, it’s easy to understand why they might feel that way. Driving through the city of Blantyre, you can see UNICEF, UKAID, and the names of various religious institutions plastered on signs outside buildings. The shiniest, tallest office building around the Polytechnic/QECH belongs to a Chinese company, and stickers with Chinese characters are plastered on the windows and doors of trucks. A good portion of the businesses are staffed by Malawians but owned by South Asians. And many of the doctors who work in the QECH pediatrics department are from other (mostly European countries). (In fact, approximately 60% of Malawi’s healthcare expenditure comes from foreign donations.)

This thought lingered with me when we visited a tea plantation right outside of Blantyre on Saturday. When we got to the entrance of the tea estate, I was surprised to find that the manager of the estate was a Caucasian woman with a crisp British accent and later learn that the estate was founded by and has continued to be owned by a Scottish family for three generations. In the video we watched before tea tasting, the tea estate was billed as a sustainable business and community with a portion of the plantation left for the natural forest, a self-sufficient bluegum tree logging and replanting operation, two clinics for the workers, and a primary school for the workers’ children. Later online investigation showed that this was the only Fairtrade certified tea plantation in the country and numerous other projects had been undertaken under the Fairtrade agenda (investment into the nearby Thyolo District Hospital, subsidized solar panels for workers, construction of roads, etc.).

Nonetheless, it’s hard to forget that the tea plantation was founded during and built off a legacy of neo-imperialism that lined the pockets of western nations and exploited the workers. And it could hardly be claimed that the plantation is an utopia now—only half the workers’ children are able to finish primary school, and food insecurity is an issue during the dry season. This exemplifies the issue that the poets at Kwa Haraba lamented and that I noticed while here: it is difficult and almost impossible to differentiate between the lingering effects of colonialism that put Malawi in this position and the efforts of foreign aid that attempt to improve the situation.
As a result, some people, especially many young Americans, would argue that it is better to avoid foreign intervention (and, to some extent, foreign aid) all together, at least at the national level. Although I truly do not have enough information to make judgments about the tea plantation or any of the other instances of foreign investment I described (clearly they’re not all equal), despite, or perhaps due to what I’ve seen here, I strongly believe past mistakes do not excuse in current inaction. While the ultimate goal is a Malawi that is truly independent from foreign influence, in the meantime, we, as an interdependent global community, have a responsibility to help Malawi and other countries like Malawi get to that point.
Part 2: Scales of Change
I fully admit that the last part of my blog was a statement of lofty thoughts and aspirations that I personally can do very little about. However, the importance of differentiating between ultimate goals and current realities has also been impressed upon me on a smaller, more personal scale recently.
As I was walking through the hospital grounds to lunch from the Rice 360 CPAP office one day last week, a man stopped me and telling me that his brother was being discharged and that he needed 2000 kwacha to pay for the minibus trip from QECH to their home in a village. I didn’t know what to do. The other interns and I had encountered people asking us for money before, and we had discussed it extensively. We talked about how giving people on the street money ultimately perpetuates an unsustainable system since it incentivizes them to keep coming back to the random people on the street instead of seeking more long-term aid from nonprofit organizations or government agencies and, consequently, prevents the social issues from garnering the attention they need. For the most part, I believed this, but, in that moment, I realized the flaws in this perspective.
I knew that transportation was a major barrier to access to healthcare services, even in the United States. For instance, during my Alternative Spring Break on maternal mortality in Texas, I learned that a major reason that pregnant women missed prenatal appointments (putting them at increased risk for maternal mortality) was that they could not bring their other children to these appointments using Medicaid covered transportation. (Though this has changed during the last state legislative session.) How could I blame that man for his country not having adequate public transportation to health facilities when this was so recently still a problem in Texas, which has exponentially more resources than Malawi?
I ended up giving him the money. (I’m aware that he may not have been truthful, but I choose to believe otherwise.) In the end, 2000 kwacha was not a lot of money to me, and while I may not have contributed to improving rural healthcare access or the public transportation system, the money allowed that man and his brother to return home after receiving the healthcare they needed.
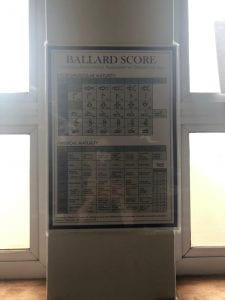
This realization about the difference between long-term sustainable change and short-term measures led me to decide to pursue a side project I had been thinking about. Seeing the Ballard Score poster, which was really a sheet of letter sized paper with the diagrams in black and white, in the NICU at QECH made me want to make a larger, laminated, and colored poster to at least match the other poster in the ward. However, I kept going back and forth about whether I should do this initially. A larger poster really doesn’t change the fact that the Ballard Score to difficult to use and that nurses don’t like performing it. Nonetheless, in my last blog, I talked about how, even in the best case scenario, a Ballard Score training program and assessment app would take years to implement. In the absence of a better training system or a better method of gestational age determination, at least a better poster would make it easier for nurses and doctors in the cases where the Ballard Score is used.
After corresponding with Prince (the nurse at QECH who works with Rice 360) and getting approval from the ward in charge to post the poster, I ultimately made four copies of 11 x 17 inch poster with a colored coded version of the Ballard Score diagram to hang in the NICU, the low risk area, and the Kangaroo Mother Care ward. While this poster clearly doesn’t make any meaningful, large scale change, I’m happy to have helped the nurses of one ward in one hospital in a small way. This week has been a valuable lesson in distinguishing between overarching aspirations and immediate measures and understanding the importance of contributing to both.
Sources:
https://mwnation.com/health-budget-at-donors-mercy/
https://www.fairtrade.org.uk/Farmers-and-Workers/Tea/Satemwa-Tea-Estates-LTD