Moni, Muli Bwanji! These past couple of days have gone by in blur! We’ve been working on several projects since arriving, and we’ve been slowly showcasing some of the technologies that we’ve brought along with us. However, when Americans (or other Westerners) proudly bring their new, appropriate medical technologies to a developing country, there’s kind of a hidden assumption that the hospital staff will absolutely love it right away and use it all the time. We’re absolutely no exception to making that sort of assumption, as we learned when demonstrating the oxygen flow splitter last week.
A Need for Oxygen
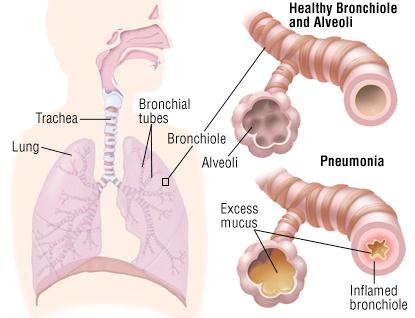
Many pediatric patients, especially those with respiratory diseases like pneumonia, need to be put on oxygen therapy. However, oftentimes developing world hospitals only have one or two oxygen concentrators (usually giving 5 or 10 L/min) for an entire ward. But most relevant pediatric patients would only need around a maximum of 2 L/min of oxygen, so the oxygen could be split into 2 or more streams. However, current oxygen ‘flow splitters’ that are used in the states are very expensive, and most hospitals in developing regions would not be able to afford them. Therefore, there seemed to be a need to develop cheaper, efficient flow splitters for these hospitals.
Many children that develop pneumonia need to be put on oxygen [1]
The Rice Flow Splitter
A team last semester at Rice was tasked with doing just that—designing a low-cost and effective flow splitter. They came up with a nice, simple design that could split a 10 L/min oxygen concentrator into 5 different ports. Each port could either give .5, 1 or 2 L/min of oxygen to the child, which could be changed by a simple rotating disk.
First Generation Flow Splitter Flow Splitter 2.0 – several improvements were added,
including a locking mechanism
Truce, Jesal and I talked a lot about their design—we thought that it was a good solution—it needed some work, like all of the designs—but it had the potential to turn into a comercializable and accessible product. We even agreed that the flow splitter would have been a really good project to be involved in, as it seemed like such a cool problem that could have such an impact.
Lack of an Actual Need for a Flow Splitter
Given our enthusiasm about the design, it was a bit disappointing when we were told by the St. Gabe’s pediatrician that “[he] would not use the device”. After the initial shock, he explained that the problem was actually quite simple to solve—he already had a well working system that connected the concentrator to copper tubing (which can be kept sterile) attached to cheap flow meters and humidifiers.
The simple flow meter+ humidifier
The St. Gabe’s system prevents numerous problems that would have arisen with the Rice flow splitter, only a couple of which I will list here:
1) The copper tubing leads directly to patient’s beds, which prevents having tangles of (hard to clean) plastic tubing everywhere in the ward.
2) Each port on the system was attached to a humidifier, whereas the Rice flow splitter would have to have the humidified air coming through the input. This increases risk of cross-contamination (as all 5 ports are connected to one humidifier) and could result in yeast/molds/bacteria growing on the inside.
3) The oxygen concentrator at St. Gabe’s is 5 L/min. The Rice flow splitter only works for 10 L/min concentrators (and would thus also not work with less than accurate O2 concentrators), whereas the St. Gabe’s system can adapt to any flow rate.
While the St. Gabe’s system isn’t perfect either, it is relatively low maintenance, works well enough and perhaps most importantly, the doctors and nurses like it.
Needing a Solution to a Different Problem
While there may be a need for flow splitters elsewhere in Malawi, there is certainly no need for one in St. Gabe’s. Even so, the St. Gabe’s system is probably significantly more likely to be useful to other hospitals in the country. However, the doctor did mention that one of their biggest problems is that the O2 concentrators are expensive and fragile, so that if one breaks, its difficult to find someone in the country who can fix it, and buying another would be prohibitively expensive. I’ve even heard similar problems with the O2 concentrators over at QECH from the Blantyre interns.
So what he really wanted was a cheap, durable O2 concentrator. This would be a significantly more difficult challenge, but one that could actually be very useful for hospitals around the country.
The O2 concentrator at St. Gabe’s
Working Together for Solutions to Actual Problems
We need to remember that the health-related problems of Malawi—and Africa—are not just one huge homogenous lump that can be fixed in a couple weeks by a few Western engineers in a comfortable office. The people here are already working extremely hard to improve healthcare, and have oftentimes come up with better working solutions to pressing issues.
Now, this doesn’t mean that we should just give up on trying to help develop appropriate technologies because our lack of understanding. Rather, it simply suggests that we listen more to doctors, nurses and community health workers on what problems they have, what they’ve tried in the past, and what they have now; as well as ramping up our efforts to collaborate with health institutions in a diverse array of low resource settings, to get a better idea of the heterogeneity of environments that exist.
Lake Malawi with Blantyre Interns!
On a fun side note, we got to spend the weekend at Lake Malawi with the Blantyre interns! We had a lot of fun going on a boat ride, seeing lots of colorful fish and ‘cliff diving’ (which was really just jumping off some rocks). It was also really cool listening to some of their experiences at QECH, as it seems to be so different than the rural setting of St. Gabe’s. I’d highly encourage everyone to check out their insightful blogs and get a better notion of the diversity of healthcare in Malawi!



The beautiful waters from our boat Truce and Emily jumping together Jesal refused to go into the water
Quote of the Day
“Pictures just don’t do this place justice” – Truce on Malawi
[1] http://www.drugs.com/health-guide/images/204871.jpg