On Thursday Jacinta and I started teaching a Medical Equipment Troubleshooting Workshop at the Malawi Polytechnic University. This class, modeled after an advanced Bioengineering Lab at Rice focuses strongly on hands-on skills. Thus, while we have powerpoints and quizzes to work with, the main thing we have needed to prepare is the equipment itself. We did not bring any machines from the States due to the fact that we wanted to make the course realistic: showcasing medical devices that actually need to be repaired here in Malawi. The Malawian health system has its own equipment care program called PAM (Physical Assets Management). They not only inventory all of the devices that come into the hospital system, but they are also responsible for maintenance and repairs. Thus to PAM we went in search of medical devices to use in our course.
On our tentative list included an Oxygen Concentrator, CPAP, Microscope, Refrigerator, Suction Pump, and Centrifuge. Oxygen Concentrators are ubiquitous in the Paeds wards at Queens, so we knew we would cover those. Also, last week we spent a lot of time repairing CPAPs, we felt confident to teach on that. As for the other devices, our coursework is strongly dependent on what is available.
After starting the class on Thursday, our mornings have been spent teaching class, and our afternoons have been spent at PAM working on repairing broken devices to use in our class. It has been a stretch outside of our comfort zones to be teaching a class to students staff who are our age or older. What we do have going for us is that we have taken the course, and we are teaching the course to Electrical Engineers: they have the technical electrical background which we aren’t as strong in, and they don’t have the physiology background that we can teach them. Acquiring devices that work still remains the biggest challenging going forward. Hope is with us, and a restful weekend.

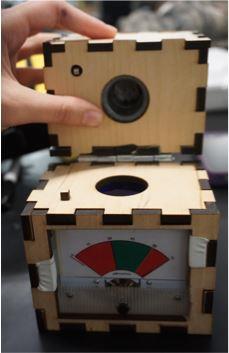
(A little improvising with props: This is basically what bronchiole tubes look like right?)