Many of the machines and materials used in the hospital are donations. This “free” equipment comes from various governments, NGOs, corporations, non-profits, or philanthropists, and oftentimes stickers or plaques attached to the machines themselves display the name of their donor. Walking through the halls of Queen Elizabeth Central Hospital, the sheer number of expatriate doctors is also surprising—many European medical students end up on rotations in Queens for a month or two as part of their training. The visible presence of donated material extends outside of the hospital walls as well. While walking the streets of Blantyre, I’ve seen University of Michigan shirts, shirts bought from local New York bakeries, South Padre island tourist shirts, and various other American clothing items. Considering that many Malawians have never left the country—and that plane tickets, food, and lodging in the US are quite expensive—much of this clothing comes from donated sources. Even the Polytechnic itself was founded with the aid of the US government back in the ‘60s.
On one hand, it’s easy to appreciate the goodwill that fueled many of these actions. It’s also easy to appreciate the positive results that the donated equipment and aid often produces—they doubtlessly save many lives daily at Queens alone.
On the other hand, it’s also easy to see the frequent disconnect between donor and recipient—the gap between intended benefit and actual need—which often results in donation and aid producing far more negative outcomes. Outside of the hospital, mounds of unusable donated equipment sits forgotten in dimly lit corners. Hundreds, if not thousands of dollars of equipment is wasted when donations are given without replacement parts, without a plentiful stock of consumables, without user manuals, or without a need. Sometimes, lack of understanding between people, cultures, and institutions results in an incredibly sad waste of resources in a place where proper resources are direly needed. For expatriate doctors, there are ample misunderstandings and frequently an inability to transfer practices that impede proper treatment; it can be difficult to use methods learned in high-resource settings to heal patients in low resource settings effectively, in a way the patient is comfortable with, and in a way the hospital can support.
Even donations as seemingly harmless as T-shirts can cause damage. Free clothing puts local tailors and textile manufacturers out of work; free shoes harms local providers of rubber and textile, and the businesses of craftsmen. Money flow decreases, local markets can be harmed, and a dependence forms. In the event of donor fatigue, recipients are often left worse off than before donors intervened.
These negative consequences have their foundation partly in a misunderstanding between people, countries, and cultures. Considering that groups born and raised in one environment are donating or providing aid to a vastly different environment, the resulting disconnect that causes so many problems isn’t all that surprising.
So, as someone who was born and raised in the US, but is currently working in Malawi and designing medical technologies for low-resource settings, I’ve thought a lot about which models of work I feel are the most sustainable, do the greatest good, and cause the least amount of unforeseen harm.
Arguably the most crucial step in sustainable work is research: the truer of an understanding we (as foreigners) can get of the context for which we are designing, the more fruitful our work will be. This research phase involves identifying needs, and defining design constraints. Without proper research and understanding, we are effectively attempting to take our model of American medical care and implant it into low-resource settings. This would waste machines, money, time, and many other resources. Instead, it’s crucial to get a firm understanding of the existing framework. This involves conversing with the doctors, nurses, and patients in Malawi to identify present needs that exist within their hospitals and have been deemed important by the actual consumer. Additionally, observing the practices and processes within low-resource hospitals and health centers helps to develop an understanding of what attributes successful technologies must possess. For example, traits such as durability and ease of use take on a much fuller meaning after spending time in the wards and seeing how technologies are handled, stored, and how much time is taken to understand them. Visiting with the engineers who fix medical machines fills out our understanding of how machines are (or are not) repaired, how consumables will (or will not) be supplied, and what materials are (or are not) available to work with. Designing medical technologies requires particularly extensive research, as the buyer (hospital), the user (doctor/nurse), the beneficiary (patient), and the repairman of each device is a different party; an understanding of each is needed to properly understand design constraints and thus design an appropriate technology.
Apart from understanding the need, the setting, and the people, the market also needs to be considered. How will the product be marketed? Who is going to buy the product? How much will they buy it for? Why will they buy it? Who will manufacture it? How will manufacturing be sustained? Is there a large enough market to support the development costs? For how long will the market exist? These questions, and dozens more, have to be taken into account. Donations will run out, and often do little to support local economic growth; on the sustainability scale, donations rank pretty low. Alternatively, a thorough understanding of the technology’s market makes the product potentially sustainable.
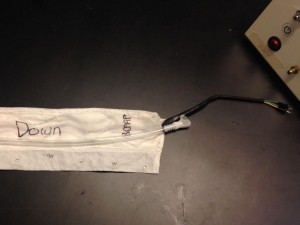
Once the need has been identified, the constraints defined, and the market considered—and after all are well understood—a device is ready to be built. While these devices often have their high-resource counterparts (expensive machines that address the same health problem in high resource settings) designing a new technology is more complex than just removing the bells and whistles from these more costly machines. Instead, the design process often starts over. Too much changes with the different settings, and the required attributes of the two devices are too varied to simply adapt an existing tech to a new environment; an altogether new device needs to be created.
Which brings us to the designers, the engineers. The four Malawian interns will always have a deeper understanding of this country than any of the Rice interns will ever hope to have. As a result, their potential to design appropriate technologies for Malawi is great. As Rice interns, we bring other strengths to the table, and our backgrounds provide us with a perspective that is also important to the process. However the partnership between groups shouldn’t end with the research phase of the design process. If patients, hospitals, doctors, and nurses from low-resource settings are involved in understanding the problem, so should be local engineers in solving it.
Luckily, we are involved in a program currently that addresses most of these concerns. Rice’s relationship with Queens is unique, and we consistently get valuable feedback from those in the wards. Interns are here every summer, and multiple faculty members work here year round. There are Malawians employed to help run the bCPAP trainings and the clinical trials. Additionally, the relationship with the Poly and Poly engineers is growing, providing even more opportunity for sustainable, appropriate, and constructive work.